
Children born with PRS have several treatment options. We are parent advocates for a non-invasive treatment called the Stanford Orthodontic Airway Plate (OAP).




We get it. Your beautiful child is born, and in many cases, whisked away by doctors to the NICU. You’re scared for their life and searching for answers. Perhaps your medical team is recommending a Mandibular Distraction Osteogenesis (aka MDO, Jaw Distraction or JD), a tongue-lip adhesion or tracheostomy. You may even feel a sense of pressure or urgency by your medical team to continue with one of these highly invasive treatment methods.

As parents of babies born with Pierre Robin Sequence ourselves, we’ve felt your pain. While invasive surgery is typically the only option presented, there is a non-invasive treatment called the Stanford Orthodontic Airway Plate (OAP). This treatment is not only more natural, but will get you discharged sooner so your child can thrive in their home environment.

Where most of the invasive treatment options only repair one aspect of PRS, the OAP works to heal all 3 attributes:
With the tongue out of the way, OAP babies see their cleft palate natrually begin to close, making the eventual cleft palate repair much easier.
You can connect directly with Stanford Children’s Hospital by clicking this link
Alternatively, you can click “Contact Us” below, and we can help you get you in touch with the Infant Orthodontics Manager for the OAP Program.
They will ask you for pertinent medical records to help determine if your child is a candidate for the OAP program.
Dr. Choo is the incredibly talented doctor behind the OAP, and the only doctor in the USA offering this treatment option. She is a neonatal craneofacial airway orthodontist and has a unique experience and understanding of PRS.
She will speak with you and answer any questions you may have. Once determined your child is a candidate, your hospital (if still in patient), Stanford and your insurance will coordinate together.
If your child is still in patient, you will likely need a medical transport from your current hospital to Stanford. This often includes a medical flight.
If your child is already discharged, you may choose to travel by commercial airline to see Dr. Choo’s team prior to admission.

Dr. Choo is busy at work documenting all her research. She has already published several papers documenting all the benefits of the OAP, and has many more in the pipeline. We have also gathered interviews, presentations and other items that may be helpful to you.
P.S. This may be very helpful to your child’s current medical team and/or insurance company!
It is an ‘orthodontic retainer’ that is removable and allows babies to breathe through the nose and feed by mouth. No surgery is needed for this treatment.
The oldest an OAP patient can be is 12 weeks old.
That said, the ideal starting time for treatment is between 2 and 6 weeks old.
Due to the fact that the OAP treatment is all about changing the baby’s lifestyle from what they are used to from birth to what they need to for normal craneofacial function and growth, babies 7 to 12 weeks old may still be considered, but the older the baby gets, the more resistance to initiating treatment is expected.
Yes! Stanford has created an OAP Program headed up by Dr. Choo. You can check out their website and full details at this link: https://www.stanfordchildrens.org/en/services/orthodontic-airway-plate.html
There are multiple nonprofit organizations that are specifically created to help patients who need medical care outside of their local area. Here are a few to look into:
Follow-up frequency varies depending on the baby’s clinical complexity. After an inpatient hospital stay of usually 2-3 weeks, parents are taught how to handle the OAP at home. When the parents feel competent in handling the OAP, then the patient is discharged home with the device. After the discharge, the family will be scheduled to return to the orthodontic and aerodigestive clinic at Stanford for outpatient visits every 3-6 weeks.
The time that the child will need the OAP depends on their clinical complexity. The average length of time with the OAP (from device delivery to graduation) is 3.5 months with the range of 3 weeks to 6 months.
As of April 2024, 29 babies were treated with the OAP and all avoided jaw surgery. One additional baby, who was later determined to have a undiscovered neurological condition did not tolerate the attempted treatment with the OAP.
When the OAP is tolerated well by the baby during the hospital stay, none of the babies needed any airway surgery afterwards. If the baby also has a cleft palate, the cleft repair will occur in the following months (typically done at your local children’s hospital).
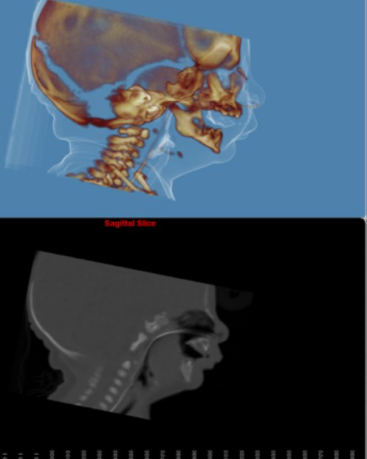
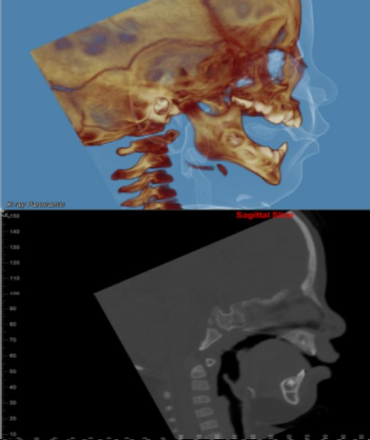
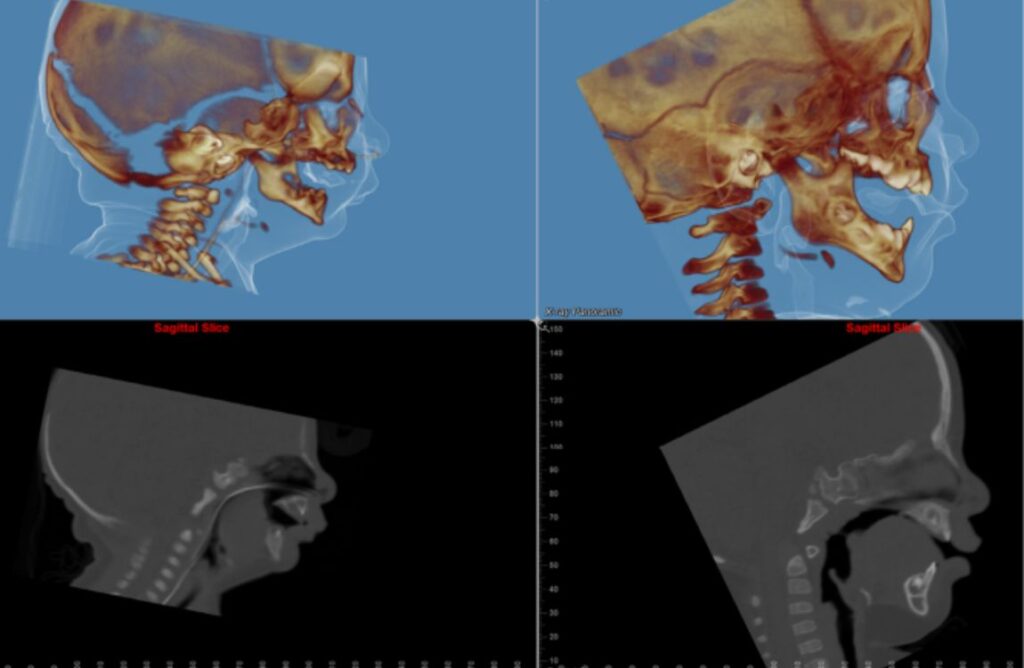
Sleep tests are done at several points before, during and after treatment. The first test is done prior to the OAP being delivered. The second one is done a few days after the delivery of the OAP (while inpatient), the third is done midcourse of the treatment (exact time varies), and one is done about a month after OAP graduation.
If your child has a cleft palate, repair surgery is typically done when the baby is approximately 12 months old. The baby will have graduated from OAP several months prior to the cleft palate surgery. The OAP often reduces the size of the cleft palate prior to the cleft palate surgery, making the surgery easier to complete.
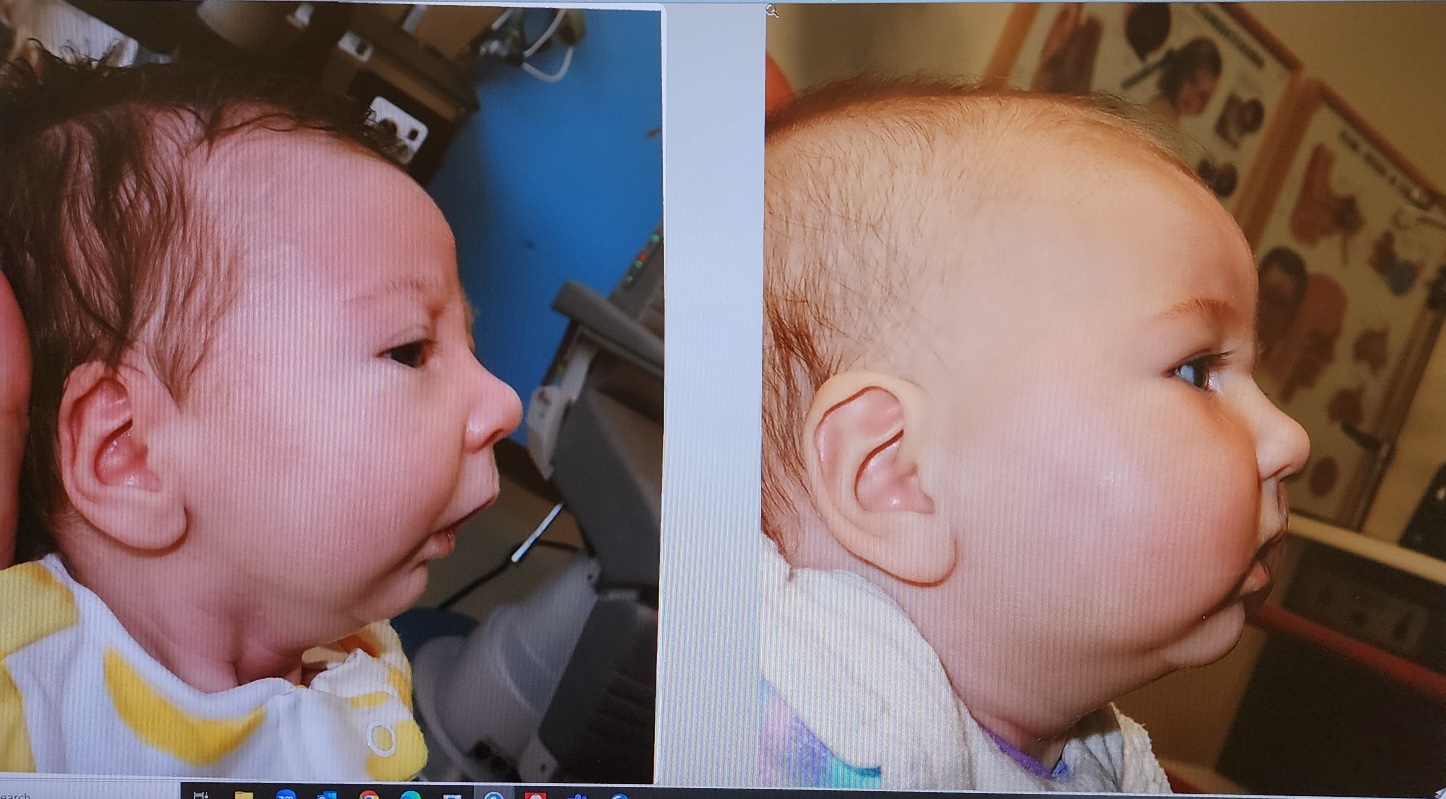
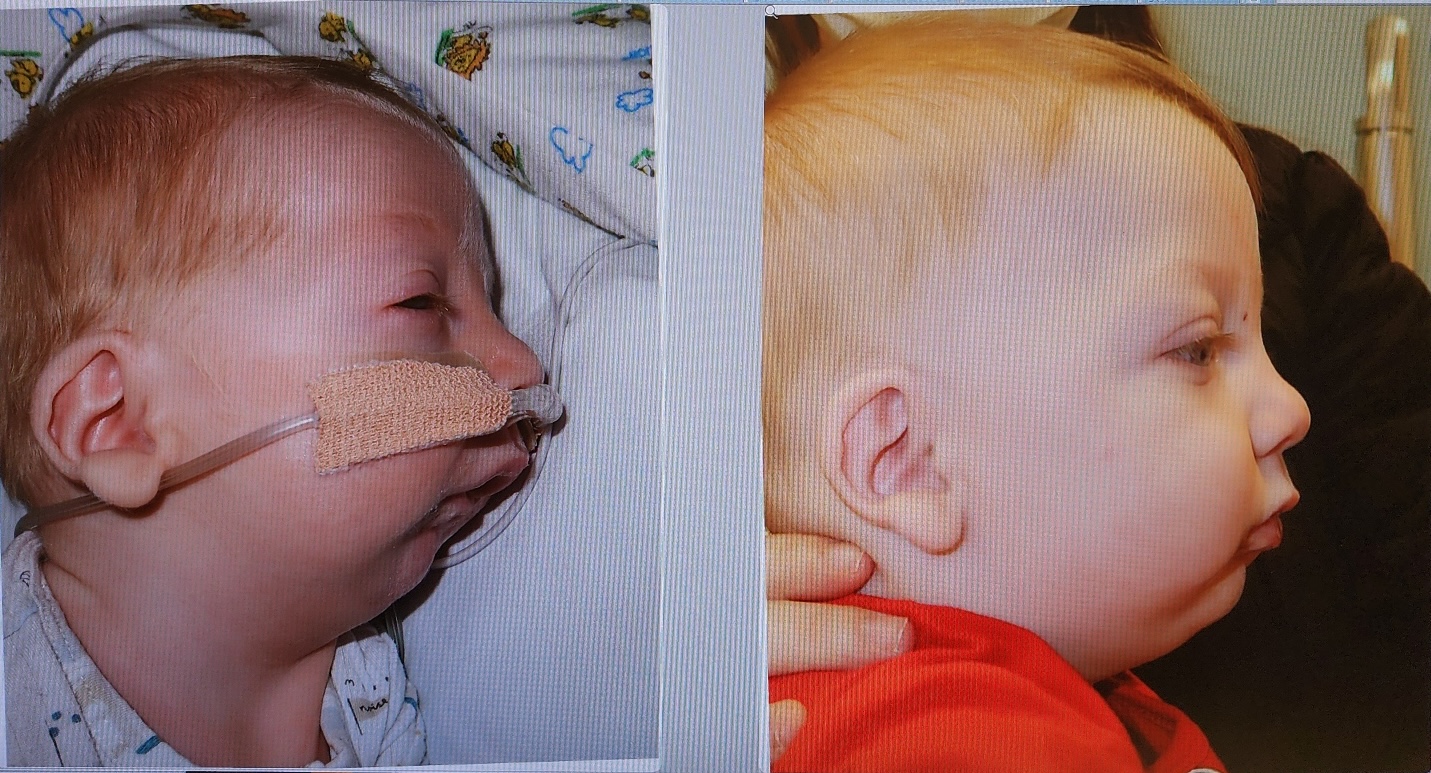
HOAP for PRS was founded by two families – one from Ohio and another from Southern California – who have been exactly where you are. Our children were born (unexpectedly) with P.R.S. in 2022.
After doing research on non-invasive treatments for P.R.S., we stumbled across Dr. Choo’s OAP Program at Stanford University. We each have our own stories on how we ultimately got our babies to Stanford, but both our boys started OAP treatment one day apart.
After experiencing the OAP treatment and Dr. Choo’s dedication to P.R.S. babies first-hand, we knew we had to help get more P.R.S. babies to Dr. Choo. We landed on starting HOAP for PRS as a way to (1) raise awareness/educating about the OAP treament (2) support parents considering & going through the OAP treatment and (3) advocating for the OAP treatment to ultimately become a standard options for babies born with P.R.S. no matter where they are in the country.
You may have noticed “HOAP” is a strange spelling for “Hope.” What does it mean? We were all encouraged by the benefits of the OAP to not only fix the immediate effects of PRS, but also the long-term effects that many PRS children face later down the road. Because of that, we wanted to convey that the OAP heals PRS, which led us to the concept of “healing with the OAP,” which led to us naming the organization: HOAP for PRS.
We love having people join us on this journey! If you share our mission and want to be a part of what we’re doing, click the “Contact Us” button and let us know.



HOAP for PRS’ mission is to give parents of PRS babies a place to answer the questions they may have about the OAP and provide them with a support system as they receive treatment. If you would like to speak with a parent whose child has been treated with the OAP, click “Contact Us” below to get started:
We are grateful for your generosity and support in helping babies avoid surgery with Dr. Choo’s game-changing treatment. 100% of your donations go to our efforts to provide education, awareness and support for the OAP. HOAP for PRS is a 501(c)3 non-profit organization and all your donations are fully tax deductible.
You can donate in the following ways:
Make payable to: HOAP for PRS
Mail to: 13131 Brittany Woods Dr.
Tustin, CA 92780
Find our Zelle account by email: hoapforprs@gmail.com
COMING SOON!